Introduction
�
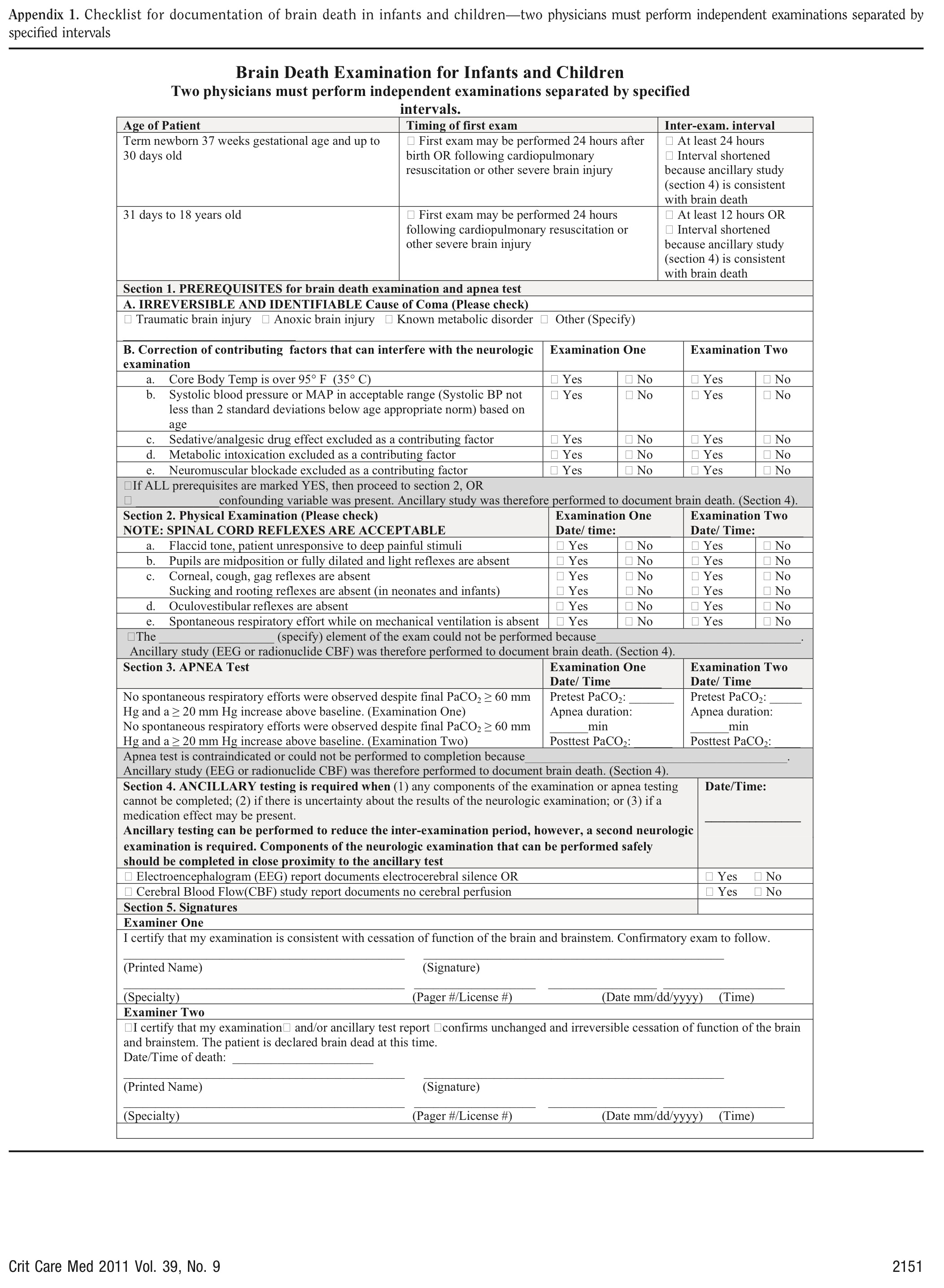
The diagnosis of Brain Death in children is generally regarded as being more difficult than in adults and there is considerable variation in the exact protocol followed in different countries, and even between different states in the same country. Nevertheless, the diagnostic procedure is essentially by clinical examination.
�
The following guidelines are based on multiple sources, including the American Academy of Pediatrics Guidelines for the determination of brain death in children 1, 4, the American Academy of Neurology evidence based guideline update 2010 2 and the Australian and New Zealand Intensive Care Society statement on death and organ donation, 2008 3.
�
Definition
�
Brain death is defined as irreversible cessation of all functions of the entire brain, including the brain stem
�
Pre-requisites
�
The following conditions must be met before brain death can be determined:
�
�
Clinical Examination
�
The diagnosis of brain death is essentially clinical.
There must be absence of higher brain function � lack of consciousness
There must be absence of brain stem functions
�
�
|
Clinical testing |
Test procedure and response |
Comments |
|
Coma |
Apply noxious stimuli in the cranial nerve distribution and all four limbs and trunk. There should be no motor response |
See note below |
|
Pupillary light reflex-cranial nerves II & III |
Shine a bright light into each eye and look for pupillary constriction. There should be no pupillary constriction |
Pupils must be ≥ 4 mm in diameter. A magnifying glass may be used, if required. Use of anti-cholinergic drugs, such as Atropine, can cause pupillary dilatation |
|
Corneal reflex � cranial nerves V & VII |
Touch the corneas with soft cotton wool. There should be no blinking or withdrawal reflex |
Touch only the lateral aspect of the cornea to avoid damage |
|
Absence of movement of the bulbar musculature � cranial nerves V & VII |
Apply deep pressure over the condyles at the temporo-mandibular joints and over the supra-orbital ridges. There should be no grimacing or facial muscle movement |
� |
|
Oculo-vestibular reflex � cranial nerves III, IV, VI & VIII |
Inspect the external auditory meatus with an otoscope to make sure that the ear drum is visible and intact � if required, clean any cerumen before proceeding. Elevate head to 30o and place in the neutral position. Instill 20 � 50 ml of iced water into the ear canal with a syringe. Hold both eyes open and observe for at least 1 minute. There should be no response � both eyes should remain in the mid-position. Wait 5 minutes and repeat test in the other ear |
Fracture of the skull base or petrous temporal may obliterate the response on the side of the fracture. |
|
Gag reflex � cranial nerves IX & X |
Stimulate the posterior pharyngeal wall on both sides with a tongue depressor. There should be no gag response |
May be difficult to examine in orally intubated patients |
|
Cough reflex � cranial nerve X |
Stimulate the trachea with a suction catheter. There should be no cough |
� |
|
Flaccidity |
Evaluate all extremities by passive range of motion (unless contra-indicated). There should be flaccid tone and no spontaneous or induced movements |
See note below |
�
NOTE
Observations that are compatible with brain death
�
The following observations can be present in brain death
�
�
Observations that are incompatible with brain death
�
The following observations are incompatible with brain death:
�
�
Number of tests and who should perform them
�
Two examinations (including two apnea tests) should be performed, separated by an interval.� A different Consultant Physician who is taking care of the child should perform each clinical examination. These physicians should have specific expertise and experience in performing such assessment and can include Pediatric Intensivists, Neurologists, Anesthetists, Neurosurgeons or Pediatricians. The same individual may perform the apnea tests. In case the testing is being performed for the purposes of organ harvesting, additional requirements from the individual State Governments may apply (such as pre-registration and authorization of the physician performing the tests).
�
Demonstration of apnea
�
The role of the apnea test has been questioned recently5. Nevertheless, it continues to be a part of the Brain Death testing protocol in most countries at this time. The apnea test must be performed twice (as part of each clinical exam), but may be performed by the same individual � preferably the physician who is managing the patient�s ventilator. The following section describes how to perform the apnea test.
�
The same pre-requisites apply as for performing the clinical tests � i.e. the patient should not be hypothermic, hypotensive or have a serious metabolic or endocrine disturbance. Additional contraindications include a high cervical spinal cord injury or very high oxygen / ventilatory requirements that will result in the inability to disconnect safely from the ventilator. If the apnea tests cannot be performed safely, then an ancillary test must be performed to determine brain death.
�
�
Response: In a brain dead patient, no respiratory efforts should be seen during the period of apnea.
�
ANCILLARY TESTS
Ancillary tests are not routinely required to determine brain death and are not a substitute for the clinical examination. However, they may be used in specific situations:
�
�
A number of ancillary tests are available.
�
EEG
A digital EEG should be performed by a technician who has experience in performing EEG�s for the purposes of determining brain death. In general, the sensitivity should be increased to 2 μV, the high frequency filter should be set above 30 Hz and the low frequency filter set not above 1 Hz. A minimum of eight scalp electrodes should be used. The EEG should demonstrate a lack of reactivity to intense somatosensory and audiovisual stimulation.
�
TESTS TO ASSESS INTRACRANIAL BLOOD FLOW
�
The purpose of these tests is to show that there is no flow in the intracerebral vessels, due to occlusion of the vasculature by cerebral edema. The various techniques by which intracranial blood flow can be assessed include four vessel cerebral angiography, Radionuclide imaging, CT angiography, Magnetic Resonance angiography and Trans Cranial Doppler ultrasonography. Of these techniques, four-vessel cerebral angiography is regarded as the gold standard and involves direct injection of contrast medium into both Carotid arteries and both Vertebral arteries.
�
Of all the confirmatory tests mentioned above, EEG is the most easily available test. Radionuclide cerebral blood flow assessment is also acceptable � the remainder are time consuming, not easily available, not always standardized, may require shifting an unstable patient and, in some cases, expensive.�
�
Any one of the following tests may be used (depending on availability) when an ancillary test is required:
�
TIME COURSE OF TESTS FOR BRAIN DEATH
�
�
Table 1 below gives the time gap between the clinical tests.
�
|
Age |
Clinical tests |
Interval between tests |
Ancillary tests |
|
Term new born (> 37 weeks gestational age to 30 days |
As adult |
24 hrs |
If required |
|
31 days � 18 years |
As adult |
12 hrs |
If required |
Transplantation of Human Organs & Tissues Rules �2014 �on Pediatric Brain Death and Apnea Test
The Indian law has the following in the Form no 10 for Brain Death �Certificate �
The minimum time interval between first and second testing will be six hours in adults. In case of children 6 to 12 years of age, 1 to 5 years of age and infants, the time interval shall INCREASE depending on the opinion of the above Brain Stem Death experts. �
Authors:
Dr. Bala� Ramachandran, Consultant and Head of the Department of Intensive Care & Emergency Medicine, Kanchi Kamakoti CHILDS Trust Hospital, Chennai [email protected]
�
Dr. Krishan Chugh, Head of the Department of Paediatrics, Sir Gangaram Hospital, Delhi [email protected]
�
Dr. Sunit Singhi, Head of the Department of Paediatrics, Post Graduate Institute for Medical Education and Research, Chandigarh [email protected]
�
Dr. Praveen Khilnani, Consultant Pediatric Intensivist, BL Kapur Hospital, New Delhi [email protected]
�
Dr. V. Viswanathan, Consultant Pediatric Neurologist, Kanchi Kamakoti CHILDS Trust Hospital, Chennai [email protected]
�
Dr. Joseph Mathew, Consultant Neurosurgeon, Christian Medical College, Vellore, TN [email protected]
�
Dr. Soonu Udani, Consultant Pediatric Intensivist, Hinduja Hospital, Mumbai [email protected]
�
Project Coordinated by
Dr.Sunil Shroff, MOHAN Foundation
�
Correspondence to:
�
Dr. Bala Ramachandran
PICU
Kanchi Kamakoti CHILDS Trust Hospital
12A Nageswara Road
Nungambakkam
Chennai � 600 034
REFERENCES
�